Written by Angela Attwood and Maddy Dyer
COVID-19 impact on research
The coronavirus (COVID-19) pandemic has forced millions of us to embrace remote working, and researchers are no exception. Universities are closed and face-to-face research with human participants has been temporarily halted. This has created challenges for our research, and laboratory and field studies are particularly affected.
As part of a large research group at the University of Bristol, we had to respond to this new situation and develop contingency plans for our research. Our first step was to review ongoing research and identify which studies could be suspended. We were fortunate on two counts: 1) we were able to put data collection on hold for many of our studies because there was enough flexibility in our planned completion times, and 2) we were able to stay busy with other work (such as analysing or writing up data from completed studies or developing new grant applications).
In all honesty, we would probably have stopped there with our contingency plans if it hadn’t been for one study that did not have this flexibility. This study investigates smokers’ experiences of switching to e-cigarettes, and requires participants to vape and complete various tasks across a two-week period. If we weren’t able to deliver on this study by a fixed deadline of the end of 2020, the funding would be withdrawn and one of our research staff would have been out of work. This forced us to think again…
Challenges and opportunities
There have been more challenges than opportunities in the context of the COVID-19 outbreak. However, one thing this global crisis has encouraged is innovation and creativity. We responded to the pressing need to complete this project by adapting our protocol so that the study could be run remotely (with no face-to-face communication). Some studies can move onto online platforms (and some of our changes include the use of online surveys), but our study involves participation over a two-week period with multiple “visits” and the use of electronic cigarettes. This required substantial adaption of the study methods (see below for some examples), but we were able to produce a comprehensive revision that retained the necessary components to ensure valid testing of our original research question.
We had to overcome several practical challenges, such as how to screen participants for smoking status and pregnancy. In the laboratory, we typically verify smoking status using a carbon monoxide (CO) breath monitor – equipment that cannot be used during lockdown. To overcome this, we replaced the CO monitor with a cotinine urine test, which verifies smoking status by detecting a metabolite of nicotine in urine. These are dipstick tests that participants can take themselves and we verify the outcome via a video call by asking them to show us the used dipstick.
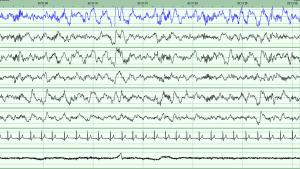
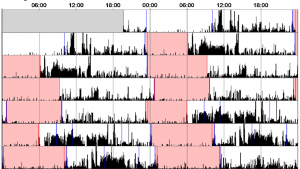
Another challenge was how to safely deliver the e-cigarettes, e-liquids, and screening tests to participants. We are doing this via post (using pre-paid postage), with carefully constructed information packs and cleaning instructions. All test sessions that collect primary outcome data are now taking place online. This includes a cue reactivity procedure that participants are led through via pre-recorded instructions that link to our online study materials. We are also exploiting ecological momentary assessment methods (daily messaging via mobile phones) to collect real-time data across the test weeks, and all face-to-face communication has been replaced with phone and video calls. We worked closely with our faculty research ethics committee and university IT services as we developed this protocol to ensure any new ideas were feasible and ethically sound (or to identify problems early and seek alternative solutions).
Our aim was to complete a project that otherwise would not have been possible. However, the important learning point was that in developing essentially what was an “emergency response” protocol, we have unlocked other important benefits. Before the COVID-19 outbreak, our biggest challenge was recruiting participants (we require smokers who are willing to abstain from smoking for one week!). As with all university-based research, we often rely on opportunistic recruitment that means recruiting from the local area (i.e., people who can easily attend the laboratory sessions during university opening hours), and our samples often comprise a relatively high number of students. This not only means we have difficulty recruiting, but that our samples are not always representative, and our results may not generalise to the wider population. This new model of working means we have no geographical restriction (as long as the post delivers and there is Internet provision – we can collect data!), hugely improving our reach and the diversity in our participant samples.
Another benefit is that data are collected in more naturalistic settings (although this comes with a loss of control that needs to be considered or may not be appropriate for some studies). For studies that require participants to attend multiple sessions, it is also likely there will be lower attrition (i.e., fewer drop-outs) as there is less burden on participants to travel to a testing laboratory.
This has not been an easy transition (although we will certainly be well equipped to do it again if we need to). It has been time consuming, and some aspects of the study were simply not possible in the context of the fixed time constraints and funding in place, and without the laboratory facilities. The utility of this approach needs to be considered on a case by case basis. But, for our study, it was doable. We are only at the start of this process – the study will be running throughout 2020 and we look forward to the ongoing challenge and reflecting on how we can optimise this process in future.
The important take-home message is that remote research is not something we will discard after the COVID-19 restrictions are lifted. We will refine these methods and embrace the benefits they offer. Remote research will not be an emergency response option only, but instead it will be an integral part of our research toolkit.
If you are interested in finding out more, please visit our website:
http://www.bristol.ac.uk/psychology/research/brain/targ/participants/smoker-experience-ecigs/
You can also follow us on Twitter: @BristolTARG @AngelaAttwood @MaddyLDyer